What Is A Gram Stain?
The gram staining procedure is a test which the laboratory performs in order to differentiate and classify bacteria.
What Is The Purpose Of Gram Staining?
The purpose of the gram stain test is two-fold.
The first purpose for gram staining is so that laboratory staff will have initial criteria for choosing an appropriate algorithm and choosing the appropriate confirmatory tests. For example, when an organism is identified as gram positive, the next test to run would be a catalase test. But if it was gram negative, an oxidase test would instead be chosen.
The second purpose for gram staining is to guide antimicrobial therapy. By identifying the type of bacteria in a clinical specimen, the doctor is better able to choose effective antibiotics to give to the patient to fight the infection. Some drugs are more effective on gram positives, while others are better for gram negatives, yet some antibiotics like Ciprofloxacin are considered “wide-spectrum” and can kill both classes of bacteria.
Gram Stain Specimen: Initial vs. Colony Growth
–Initial Gram Stain (IGS): An initial gram stain will be done using whatever specimen has been sent down to the lab. This could be a wound swab, throat swab, CSF, or urine to name a few. These initial results at least give the doctor a general idea of what class of bacteria could be infecting the patient, since the agar plates haven’t been inoculated, incubated and tested yet. For example, even without an organism I.D., an initial gram stain that is showing gram positive cocci in clusters, in addition to the patient’s signs & symptoms, may give the doctor enough evidence to presumptively treat for Staphylococcus species. Consequently, they may start medications that are effective for treating Staphylococcus species.
–Colony Growth: After the agar media has been inoculated and incubated, gram stains will be performed again the next day using well isolated colony growth from the agar plates. These are often easier to read than the initial gram stain specimens since the colony growth is much more concentrated. However, due to this extra concentration, it does become necessary to dilute the colony with distilled water on the slide to ensure that the smear is not too thick. If the smear is too thick and presents a “milky” appearance, the cells will be clumped together and make it hard to differentiate the cell arrangements.
Gram Staining Procedure
If you want to learn how to gram stain, it can be done by following these next steps.
Step 1- Make the smear
Initial Gram Stain: If using a liquid specimen like urine or CSF, place 1 drop onto the center of the slide. If using a swab, roll the swab onto the center of the slide in order to transfer the material into a space about the size of a quarter. Make sure to rotate it at several angles so that everything on the swab is transferred to the slide.
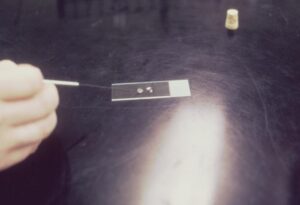
From colony growth: When using growth from a colony, open up an agar plate and select a well isolated colony with an applicator stick or an inoculating loop. For smaller colonies, you may need to pick up 2-3 colonies. Transfer the colonies to the center of a slide and add a drop of distilled water on top of it. Mix the colonies and water until they make a homogenous suspension. The suspension should be slightly turbid. If it is too turbid, add more water. If it’s not turbid enough, add more colonies.

Step 2- Fixation
Once the specimen is transferred, it must be fixed to the slide. If the bacteria aren’t properly fixed, it will get rinsed off of the slide during the staining process. There 2 methods of fixation which are commonly used are the heat method and the methanol method.
Heat Method: Using this method, involves letting the slide sit on a warmer at 60°C for about 5 minutes. Alternatively, you can pass the slide over a flame several times.
Methanol Method: Either flood the slide with 100% methanol while lying flat, or let it soak in a jar of methanol. After 2 minutes has elapsed, drain the methanol from the slide either by tilting it or taking it out of the jar. Allow it to air dry.
One of the benefits to methanol fixation is that it maintains the cell structure and morphology better than the heat method.
Now that the specimen has been added to the slide and fixed, it is time to perform the staining portion of the procedure. A gram stain kit will be necessary to perform the next steps 3 through 6. The kit contains the 4 bottles that you will need which includes Crystal Violet, Iodine, Decolorizer and Safranin. It is important to keep the bottles in order since it is crucial that they get used in the proper sequence.
Step 3- Crystal Violet
Crystal Violet is the “Primary Stain” and is what gives gram positive bacteria their bluish-violet color. When Crystal Violet is applied to the slide, all bacteria will stain a bluish-violet color, but only gram positives will retain the color at the end of the procedure due to the thick layer of peptidoglycan in their cell wall. Crystal Violet is the first bottle in the kit.
To apply, flood the slide with Crystal Violet and allow to sit for 60 seconds. Once time has elapsed, rinse with tap water gently and allow to drain off into the sink.
Step 4- Gram’s Iodine
Iodine is the second bottle in the gram stain kit and plays the role of a mordant in the process. The purpose of a mordant in the gram stain is to help bind the Crystal Violet to the cell wall.
To apply, flood the slide with Iodine and allow to sit for 60 seconds. Once time has elapsed, rinse with tap water gently and allow to drain off into the sink.
Step 5- Decolorizer
The third bottle in the sequence is a combination of alcohol and acetone named Decolorizer. This is the step which washes away any unbound Crystal Violet from gram negative cells, due to their very thin layer of peptidoglycan. This is the hardest step for beginners because a small moment of time can mean either under-decolorizing or over-decolorizing. If you stop applying it to soon, the cells will be under-decolorized and everything will look gram positive. Too late and you will over-decolorize, washing out all Crystal Violet even from gram positive cells.
For the Decolorizer stage, there is no flooding the slide for 60 seconds. Instead, while holding the slide at an angle over the sink, pour Decolorizer over it until the liquid that is running off into the sink is clear, instead of blue. Rinse gently with tap water and allow to drain off into the sink. Do not let it sit on the slide any longer than it has to, or it will over-decolorize.
Step 6- Safranin
The last bottle in the kit is Safranin and is known as the “Counterstain”. The purpose of the counterstain is to give color to the gram-negative bacteria which just had the unbound Crystal Violet washed away. This will give them a reddish-pink color.
To apply, flood the slide with Safranin and allow to sit for 60 seconds. Once time has elapsed, rinse with tap water gently and allow to drain off into the sink.
Step 7- Air Dry
Once the slide is stained, it must be allowed to air dry. You can carefully blot in order to speed up the drying by removing big droplets of water, but do not wipe the slide because this can accidentally remove the smear from the slide.
Step 8- Read the Slide
Once the slide is dry, you can now read it under the microscope. You can begin scanning on the 40x objective to find a good area of the slide which isn’t too light or too thick. Next, put a drop or two of immersion oil on the slide and observe under the 100x objective. Scan several fields until you are able to identify the cell morphology.
Gram Stain Results Interpretation
The 3 parts of a gram stain interpretation are color, shape and arrangement.
Color
-Gram positive: bluish-purple
-Gram negative: reddish pink
Shape
-Cocci: circular shaped
-Diplococci: two cocci merged together, sometimes resemble a “kidney bean” or “coffee bean” shape.
-Tetrads: groups of four cocci merged together in the shape of a square.
-Bacilli: rod shaped.
-Coccobacilli: Some organisms are a combination of a cocci and bacilli and are known as coccobacilli.
Arrangement
-Clusters: resemble clusters of grapes. Only seen with cocci and is common with Staph species.
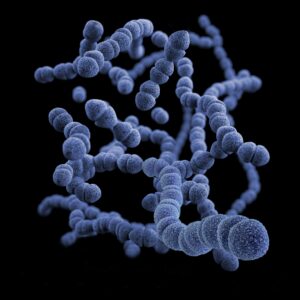
-Pairs and Chains: cells will stick together as a pair or will link together into short or long chains. Usually seen in cocci, but can occasionally be seen in bacilli. Common with Strep species. Chains will often be longer and easier to see when the stain is made from “Thio” broth.
-Palisades: Only seen with bacilli. Observed as cells lined up in a row similar to a “picket fence” or as cells lines up with each other at an angle similar to “Chinese letters”.
-Spores: spores do not react to gram staining. Therefore, they will be seen as clear ovals or spheres. Spores can last for long periods in harsh environmental conditions and are only found in certain gram-positive bacillus.
Note: It is important to consider which type of stain you are performing. If it is an initial gram stain, it is normal to see both gram positive and gram negatives, or cocci and bacilli. This is because the initial gram stain specimen source often contains mixed flora. However, if you are making a smear from a pure colony isolate from an agar plate, you should only be seeing one type of bacteria. If you see multiple, then you likely had some contamination with another isolate.
List Of Gram Stains For Most Common Bacteria
Staphylococcus Aureus
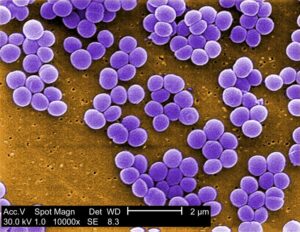
Gram positive cocci in clusters.
Staph aureus is one of the most commonly isolated bacteria in the lab. It is often used for quality control “QC” for gram positive organisms.
Staphylococcus epidermidis
Gram positive cocci in clusters.
Staph epidermidis is another commonly isolated Staph species. It is classified as a Coagulase Negative Staph, unlike Staph aureus.
Streptococcus Pyogenes (Strep A)
Gram positive cocci in pairs and chains.
Strep A, the causative organism of “Strep Throat”, shares the same gram stain as other serotypes like Strep B, C, D, F and G.
Streptococcus pneumoniae
Lancet shaped diplococci or short chains
Strep pneumoniae is the leading cause of ear infections in the world.
Escherichia coli (E.coli)

Gram negative bacillus
E coli is the most frequently isolated gram-negative bacteria. It is also commonly used in labs as a “QC” organism for gram negatives.
Enterococcus faecalis
Gram positive cocci in pairs and chains
Neisseria gonorrhoeae
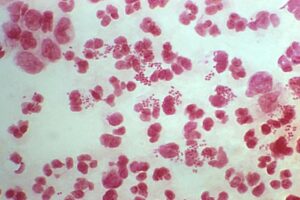
Gram negative diplococci (GNDC)
This bacteria which causes the STD gonorrhea, looks like little pink “kidney beans” or “coffee beans”. Other species which are also GNDC include Neisseria meningitidis and Neisseria lactamica.
Bacillus cereus
Gram positive bacillus in chains, spore forming.
Bacillus subtilis
Gram positive bacillus in chains, spore forming.
Bacillus anthracis
Gram positive bacillus in chains, spore forming.
This organism came to world-wide notoriety after the 9/11 attacks. Terrorists were putting spores of “anthrax” inside letters and mailing them to unsuspecting people across the U.S. causing death and sickness in several of them. Because of the hardy nature of the spore form of bacteria like this, they were able to survive and cause harm once the letters were opened.

Pseudomonas aeruginosa
Gram negative bacillus, non-spore forming
These bacteria also have a characteristic odor which is described as “grapes” or “corn tortillas”. They also demonstrate a pearly sheen when grown on sheep blood agar.
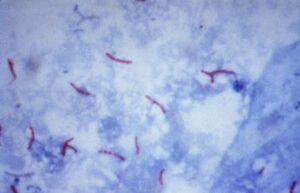
Mycobacterium tuberculosis
TB is an acid-fast bacterium (AFB), and is not responsive to gram staining. Therefore, AFB stains like the Ziehl-Neelsen technique must be used and will show M. tuberculosis as pink bacilli amongst a blue background.
Enterobacter aerogenes
Gram negative bacillus, non-spore forming.
Nocardia
Branching, filamentous, gram-positive rod.
Nocardia is weakly acid-fast and has a “beaded” appearance.
Klebsiella pneumoniae
Gram negative bacillus, non-spore forming.
Legionella pneumophila
Thin gram-negative bacillus, non-spore forming.
This organism causes a serious lung condition called “Legionnaires’ Disease” and a flu-like illness named “Pontiac Fever”.
Listeria monocytogenes
Short gram-positive bacillus in palisades. Non-spore forming.
Unlike most bacteria, Listeria is extremely cold tolerant and can thrive at very low temperatures. In fact, Listeria was the organism responsible for the Blue Bell ice cream outbreak in 2015 that killed several people.
Gardnerella vaginalis
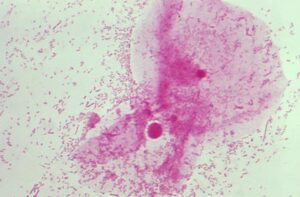
Gram variable bacillus. Non-spore forming.
G. vaginalis is normal flora of the vagina but can cause bacterial vaginosis when it experiences overgrowth. Also, G. vaginalis is often seen in clue cells, which are epithelial cells covered in bacteria.
Serratia marcescens
Gram negative bacillus. Non-spore forming.
Lactobacillus
Gram positive bacillus. Non-spore forming.
Corynebacterium
Gram positive club shaped bacillus, in palisades. Non-spore forming.
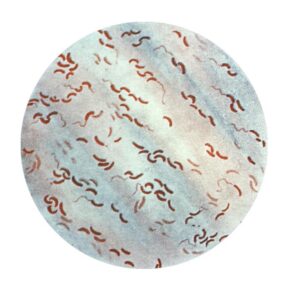
Campylobacter
Gram negative S-shaped, spiral, or curved bacillus. Resembles “gull wings”. Non-spore forming.
Haemophilus influenzae
Gram negative coccobacillus. Non-spore forming.
Candida albicans
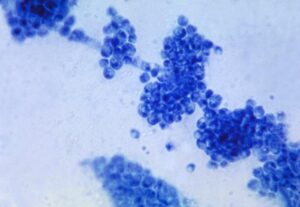
Even though this is a fungus and not a bacteria, Candida can still be gram stained and it will retain crystal violet. Due to the retention of crystal violet, it will stain as gram positive.
Because Candida is a dimorphic fungus (alternates between a yeast phase and a mold phase), the gram stain will appear differently depending on which phase it is in. While in the yeast phase, it will be visualized as round to oval circles, similar to a cocci. However, for size comparison, they will be larger than a typical coccus, yet smaller than a standard size red blood cell.
While in the mold phase, Candida will experience the growth of hyphae and will branch out into long strands or chains of filamentous growth, which often resemble long, thin bacilli.
Clostridium difficile
Gram positive “box car” shaped bacillus in pairs and short chains. Spore forming.
Proteus mirabilis/Proteus vulgaris
Gram negative bacillus.
Yersinia pestis
Gram negative coccobacilli. Closed safety pin shaped. Experiences bipolar staining where the stain is taken up unevenly, causing different portions of the cell to have color or no color.
Vibrio
Gram negative, comma shaped bacillus
Conclusion
Gram stains give the lab a starting point for confirming an organism’s identification and also give medical providers a head start for which way to direct antibiotic therapy. Gram staining is an invaluable tool for the field of microbiology.











