The short answer is that a type and screen tells you the blood type and antibody status of a person , whereas a crossmatch tells you whether a particular unit of blood is compatible with that person. Each of these tests are required before red blood cell units can be transfused. Let’s dive deeper into detail for each of these pre-transfusion tests below.
What Is A Type & Screen?
The “type and screen” blood test determines the prospective blood recipient’s blood type as well as determining whether the Rh status is positive or negative and whether there are antibodies present or not. This is the bread and butter of pre-transfusion testing and is the most common panel run in the blood bank.
Specimen of Choice & The 72-hour rule
The most common specimen of choice in the modern blood bank is the 7 ml pink top EDTA tube, although red top “clot tubes” may still be used in certain facilities.
Per AABB standards, type and screen specimens are only good for 72 hours if blood products are needing to be transfused. If a patient’s specimen has exceeded the 72- hour mark a new tube must be drawn in order to use for any blood product issuing.
Moreover, there is an additional requirement which often gets overlooked. If a patient gets discharged and is then readmitted, a new specimen must be redrawn, even if it has been less than 72 hours since the last one.
The reason for such strict specimen requirements is to ensure that the recipient’s blood has had time to present any significant changes that may affect compatibility with blood products. The ABO/Rh will rarely change during this timeframe, unless there is history of a recent massive transfusion. Rather, it is clinically significant antibodies that have more of a risk of appearing, even in a short timeframe like 72 hours.
The Re-type Specimen
If type specific blood products are needed for transfusion a second ABO/Rh specimen called a “Re-type” must be drawn as well. This tube must be drawn at a different time (generally at least 1 minute apart from the prior tube). Once the type and screen tube is drawn a new label will print out, prompting the draw of the second tube for the re-type. The re-type process helps minimize the risk of patient identification errors and ensures that the corresponding results truly belong to that patient. The theory is that a tube can get mismatched from its patient fairly easily if proper labeling procedures are not used. But the probability of this happening twice with the same patient, should have its odds reduced if the re-type system is properly utilized.
Blood Typing
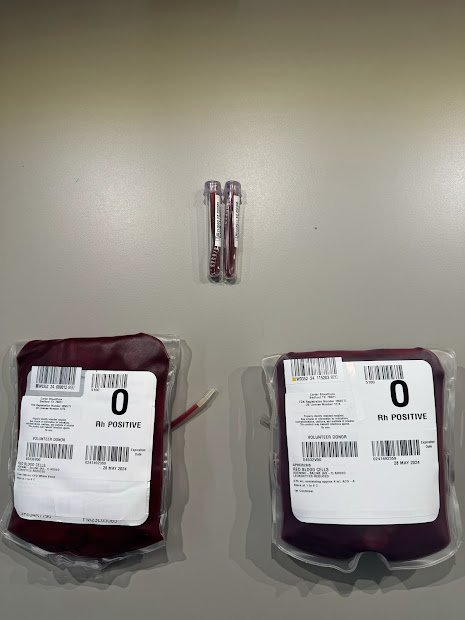
The “type” portion of the type and screen test determines the patient’s ABO and Rh status. The ABO test tells which antigens are on the red blood cells and determines if somebody is type A, B, AB or O. Likewise the Rh test tells whether a person has the D antigen on their red blood cells, classifying them as either Rh positive or Rh negative. Knowing the ABO/Rh of a patient is important because it gives healthcare teams the edge of knowing what blood will be compatible if a transfusion becomes necessary.
The actual ABO/Rh testing procedure involves mixing a 2-4% suspension of patient red cells with Anti-A, Anti-B and Anti-D antisera (front-type testing) in order to detect any ABO/Rh antigens on the red cell surfaces. Patient serum is also mixed with Type A and Type B reagent red cells (back-type or reverse testing) in order to confirm the front typing. ABO/Rh testing is only one phase and is performed at room temperature. It can be completed in about 5 minutes if done on the bench, or about 15 minutes if using automation like the Ortho Vision analyzer. At the end of ABO/Rh testing, you will have a result such as O positive or O negative, etc. to classify the patient’s blood type with.

Antibody Screen
The “screen” portion of the type and screen test tells whether there are any antibodies in the patient’s serum or plasma. There are many antibodies out there, but only a handful which are clinically significant. Rh, Kell, Duffy, Kidd, Lewis and MNS are the most common families of important antibodies.
The antibody screen is run by mixing patient serum or plasma with a 3-vial set of pooled reagent screen cells. If any of the screen cells come up positive, then the serum/plasma must then be run against a more comprehensive full set of pooled reagent cells in order to identify the antibody. Unlike the typing portion of the panel, the antibody screen and ID both get tested at room temp as well as 37 Celsius, since “cold” antibodies react better at room temp and “warm” antibodies react better after incubation. Consequently, the antibody screen will take longer to perform than the typing since you have to incubate, wash the cells, add AHG and perform Check Cells. The antibody screen will take about 30 minutes and if it makes it to the Antibody ID phase, that will add another 30-60 minutes on top of that. This turnaround time illustrates the importance of the timely submission of type and screen samples. The earlier these results can be certified, the less likelihood that it will be necessary to conduct an emergency release due to lack of a specimen and crossmatch capability.
Phenotyping of The Recipient
If an antibody is identified, the patient’s red cells need to be “phenotyped” to ensure they don’t possess the corresponding antigen to the antibody that was just identified. They should not have the corresponding antigen on their red cells, or else these cells would get attacked by that antibody. This aligns with the general rule in blood banking that you should never have the same antigen and antibody in the same person. However, if this does happen, it should trigger the tech to investigate their work for any discrepancies.
What Is A Crossmatch?
Once a patient has had their type and screen completed, they are now ready to be crossmatched. This is when the patient’s serum or plasma is mixed with donor unit red blood cells.
Crossmatch Overview
A crossmatch test will be ordered by the patient’s provider and will request how many units of red blood cells they want to have tested. Normally, this is only 1 to 2 units, although more can be requested based on the need. Based off of the type and screen results, the requested number of compatible units will be taken from inventory and put to the side. If there was an antibody identified earlier, these units would all need to be phenotyped in order to ensure they are negative for the antigen which corresponds to the antibody. Any units that are positive for the antigen would be put back on the shelf and switched with another unit, since they are not able to be used. If units are negative for the antigen, the crossmatch process can begin.
Performing A Crossmatch
To perform a crossmatch, 2 drops of patient serum/ plasma will be mixed with 1 drop of 2-4% donor red cell suspensions from the units that were just phenotyped. If the recipient has no antibodies, the tubes will be spun in a centrifuge and then the results will be read at immediate spin. However, if they have an antibody, an “extended” crossmatch must be done which gets carried thru the additional incubation, washing, AHG and Check Cell stages. If an extended crossmatch is inadvertently taken only to immediate spin, this could cause a false compatible crossmatch reaction, potentially causing a transfusion reaction later on. The blood bank must take great care to avoid missing any of these critical steps.
Crossmatch Interpretation
If there is agglutination in the tube in any phase (except Check Cell), it means that the unit is not incompatible and should not be used. This could be due to lab error, potentially requiring the lab to investigate the cause. Potential causes include, inaccurate type and screen results, wrong ABO type of chosen donor units or error in phenotyping of donor units.

If there is no agglutination seen in the tube, the donor unit is deemed compatible and is appropriately tagged with the patient info. It is typically placed on a designated “Crossmatched” shelf so that it won’t get used for any other patients. However, since the crossmatch is only valid for 72 hours from the time that the type and screen was drawn, units are returned to the shelf once this time has expired.

Do All Crossmatched Units Get Transfused?
No, many crossmatched units actually never get used. This is because there is a protocol in most facilities to have crossmatched units on standby for certain procedures, like C-sections and other high bleeding risk surgical procedures.
Closing Thoughts
For those not familiar with blood banking terminology, it’s easy to get the type & screen and crossmatch procedures confused. They are both very different tests, but at the same time they are very dependent on one another. Blood can’t be transfused without being crossmatched. While at the same time blood can’t be crossmatched unless it has a current type and screen. This system of checks and balances helps ensure that patients get the blood products they need without causing them any further harm.