– Original Photo
Published: 19 September 2023
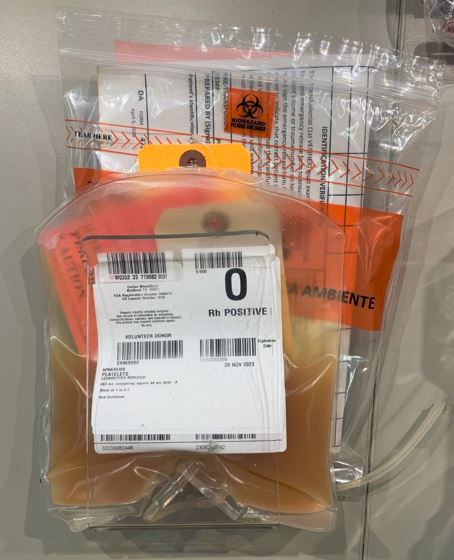
Donating platelets is vital in helping sick patients who suffer from various diseases and traumatic injuries. According to the Red Cross, someone in the U.S. needs platelets every 15 seconds. It is no surprise that about 2 million units of platelets are transfused every year. Today, we will discuss the platelet donation process as well as some other important related topics.
What Type of Patients Need Platelets
The goal of prophylactic therapy is for the patient to achieve platelet counts above 25,000/ul, although some conditions will require a higher count. The transfusion of each apheresis unit is typically expected to raise the platelet count of an adult by 20,000/ul to 40,000/ul (Davenport & Mintz).
Trauma
When someone experiences a traumatic injury like a gunshot, stabbing or motor vehicle accident, it is possible that they may lose a large volume of blood. In these instances, hospitals will usually transfuse blood products like red blood cells, fresh frozen plasma and platelets in order to replenish oxygen carrying capacity and clotting capabilities that have been reduced due to hemorrhage.
Surgery
When patients undergo a major surgery, blood loss is a common occurrence. Platelets are often needed to get these patients back to normal so they can quickly recover from their procedure.
Cancer
Patients undergoing cancer treatment like chemotherapy often experience damage to their bone marrow. This can lower platelet production and require external sourcing from platelet donors
Platelet Donor Eligibility
Donor eligibility is generally the same as for a standard whole blood donation. However, there are a few deferrals specific to platelets that can prevent you from donating temporarily.
If you have taken aspirin or other medications containing aspirin, you should not donate platelets for at least 48 hours. 48-hour deferral also applies to those taking Feldene (Piroxicam),
If you’ve taken Effient (Prasugrel), you are deferred from donating platelets for 3 days.
For Brilinta (Ticagrelor), you are deferred for 7 days from donating platelets.
If you have recently donated platelets, you will be deferred from donating platelets again for another 7 days. There is also a maximum of 24 donations allowed per year.
Platelet Count: In accordance with FDA standards, a pre-donation platelet count should be at least 150,000 platelets/microliter to donate.
How Does Platelet Donation Work
The apheresis platelet donation process follows the same general process as that of standard whole blood and plasma. However, due to the extended phlebotomy time, the platelet process will take longer, usually about 2-3 hours from the time you arrive. This extra time commitment may be a deterrent for some donors when compared with plasma and whole blood collection times.
- A person must first report to a donor center and have their records checked for any previous deferrals from previous visits.
- An interview must be performed to determine suitability based on medical history.
- A physical exam using visual assessment and vital signs measurements must be performed to ensure the welfare of the donor as well as the safety of the drawn unit for the recipient.
- Once you are deemed fully qualified to donate, you will be sent back to the phlebotomy section to have the unit drawn. How Long Does Platelet Donation Take? Due to the extended phlebotomy time, the platelet process will take longer than a standard blood unit draw, usually about 2-3 hours from the time you arrive. Ensure you have eaten a snack or light meal prior to donating to help prevent any potential adverse reactions.
Platelet Apheresis Process
Platelet concentrates are one way to harvest platelets from a donor. This is done by pooling together 6 to 8 random platelets after spinning down whole blood. However, this is not an efficient process and exposes recipients to additional donors, increasing the risk for disease transmission.
On the other hand, apheresis platelets are a much more efficient process and significantly reduce recipient exposure to only one donor. This requires the use of apheresis machines like Haemonetics, Fenwal, Terumo and Fresenius models to name a few.
Once seated, the phlebotomist will first verify your information before setting up the machine’s cassette and tubing.
When the machine is ready and a suitable vein is found and disinfected, the needle will be inserted and the machine turned on. Older techniques utilized a two-needle technique, placing one needle in each arm. However, most modern methods now use only one needle. How big is a needle for donating platelets? This will depend on what you are using, but machines like the Trima Accel uses a 17 gauge needle. This is smaller than the standard RBC collection 16 gauge needle, but still bigger than the typical 21 gauge venipuncture needle used for drawing standard labs.
Blood will be pulled into the machine tubing where it will be centrifuged down. The target component (platelets) will be segregated and retained into a special container while the red blood cells and plasma will be returned to the donor’s arm through the same tubing after being mixed with a citrate-based solution.
The blood removal and return cycles will alternate until the target volume has been collected, and depending on the target component. For reference, donating a double platelet product will take 83 minutes on the Trima Accel System, but can take shorter or longer depending on which system is used, the donor’s platelet count and whether a single, double or triple unit is being collected. Also, a single needle system will take longer than a double needle system since the draw and return cycles are occurring thru one needle instead of two.
Once the target volume has been hit, the phlebotomist will remove the needle and bandage up the donor’s arm. They will then give post-donation instructions to the donor and send them to the recovery room for refreshments if they are equipped to do so.
They will then remove the cassette with tubing and clean/reset their machine for the next donor. Next, the platelet unit will be transported back to the processing station for further handling.
Platelet Donation Side Effects
Side effects are generally mild.
Platelet Count
Plateletpheresis will lower the donor’s platelet count by 20%-30% immediately after the procedure (Kay). Fortunately, they should return to normal levels within the next 72 hours.
Pain
You will feel some slight discomfort when the needle is inserted. The needle will be a little larger than the normal venipuncture needle, so this could surprise a donor who is used to smaller needles. You should only feel this one time, however, it may be multiple times if the phlebotomist misses the vein on the first attempt.
Bruising Hematoma
You may notice pain or bruising both during and after the phlebotomy. This is often due to “traumatic sticks” where there is digging for a vein. It could also be due to a hematoma, where the needle goes through both sides of a vein and blood begins to pool, causing bruising, swelling and pain. With apheresis, this can also cause “infiltration”, where the fluids that are supposed to be returned to the donor’s vein are instead dispersed outside of the vein due to positioning of the needle bevel. Infiltration is extremely painful for the donor.
Scar Tissue
Due to the large needle size, as well as the frequent nature of platelet donations, it is fairly common to experience thickening of the skin in the needle insertion area, as well as the vein itself underneath the skin. This scar tissue is caused by the repeated trauma of phlebotomy occurring in the same spot and is the body’s way of repairing the damage. This can be prevented or reduced by avoiding the repeated use of the same vein and instead rotating between veins and different arms.
Feeling Cold
You may feel a little chilly. This is due to the fluids that are being injected back into you, which are usually not up to body temperature of 37 Celsius. Rather these fluids are typically kept at room temperature between 20-24 Celsius.
Vasovagal Response
Some donors may experience lightheadedness or dizziness either during or after the procedure. This is often due to a “vasovagal response” where the body’s heart rate and blood pressure drop suddenly due to a stressful trigger. In severe cases, this can lead to passing out. If this happens, the donor staff will take action by administering ice packs, elevating the feet, loosening any restrictive clothing and monitoring vitals until they have come back into normal range.
What To Eat After Platelet Donation
After donating platelets, it is essential to eat and drink something to replace any fluids and nutrients that have been lost in the process, hopefully preventing any adverse reactions.
Water & Juice
Water and juice should be drank to replenish any lost fluids and rehydrate the body. Caffeine and alcohol should be avoided since they can further dehydrate the body.
Sugary Snacks
These are ideal post-donation since they can help replenish any lost glucose. They should be relatively light though since they are easier to digest than a big heavy meal.
How Long Are Platelets Good For

Conventionally, platelets have a 5-day shelf life and have to be stored at room temperature (20-24C), with constant agitation. However, in June 2023 the FDA approved the use of Cold Storage Platelets. With this new variety of platelets, they can be refrigerated between 1-6C for up to 14 days, with agitation being optional. This new development was in response to an urgent need for platelets for the treatment of active bleeding when conventional platelets are not available, or practical. Sustaining platelet inventories have posed significant logistical challenges to healthcare facilities, so this advance is critical for assuring availability of platelets for patients with active bleeding.
How Much Do Platelets Cost
In comparison to red blood cells and plasma, platelets are the more expensive blood product. This was highlighted in a recent study of amount paid per blood product unit by U.S. hospitals in 2019 (Sanjida J. Mowla, 2021). According to the data, when considering the cost of 1,537 leuko-reduced apheresis platelets units, the average price was $516 per platelet unit. The average price jumps to $617 for pathogen-reduced platelets. Considering the average price of leuko-reduced red blood cells (average price of $208) and Fresh Frozen Plasma (average price of $50), platelets clearly carry the higher price tag.
Can Women Donate Platelets
Yes, women are able to donate platelets. The only time women may not be eligible to donate platelets is if they were ever previously pregnant.
This is because some women produce antibodies for Human Leukocyte Antigens (HLA) during pregnancy. These antibodies remain in the women’s bloodstream even after delivery and can cause adverse reactions like Transfusion Related Acute Lung Injury (TRALI) in future blood recipients.
The good news is that women can be tested for the presence of HLA antibodies and if they test negative, then they are cleared to donate platelets, as long as they meet the rest of the pre-screening requirements. If they test positive for HLA, they won’t be able to donate platelets, but they will at least be able to donate red blood cells.
Women are a valuable component of the transfusion community, so their ability to donate should be maintained with an HLA testing program.
Conclusion
Donating platelets is crucial in helping the medical community maintain its inventory . It is a blood component in short supply, with serious collection and storage issues to contend with. However, with recent regulatory guidance, cold storage platelets might play a key role in alleviating this dilemma, along with the loosening of several common deferral requirements which has helped to broaden the donor pool size.
References
Alternative Procedures for the Manufacture of Cold-Stored Platelets Intended for the Treatment of Active Bleeding When Conventional Platelets Are Not Available Or Their Use Is Not Practical. (2023, June ). Retrieved from FDA: https://www.fda.gov/media/169714/download
Davenport, R. D., & Mintz, P. D. (n.d.). Transfusion Medicine. In R. A. M.D., & M. R. Pincus, Henry’s Clinical Diagnosis & Management by Laboratory Methods (p. 675).
Kay, J. L. (n.d.). Chapter 8- Donor Screening & Blood Collection. In S. V. Rudmann, Textbook of Blood Banking & Transfusion Medicine, 2nd Edition (p. 225).
Mobile Reference Guide. (2012). Retrieved from Terumo BCT: https://kiosk.terumobct.com/Trade%20Show%20Documents/306620228B-web.pdf
Platelet Donation. (n.d.). Retrieved from American Red Cross: https://www.redcrossblood.org/donate-blood/how-to-donate/types-of-blood-donations/platelet-donation.html
Sanjida J. Mowla, M. R. (2021, September). Supplemental findings of the 2019 National Blood Collection and Utilization Survey. Transfusion, 61(S2), S11-S35. doi:https://doi.org/10.1111%2Ftrf.16606
Title 21, Volume 7; PART 640 — ADDITIONAL STANDARDS FOR HUMAN BLOOD AND BLOOD PRODUCTS. (2023, June 7). Retrieved from FDA: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=640.21#:~:text=(d)%20If%20you%20are%20collecting,%5DL)%20before%20plateletpheresis%20begins
Trima Accel Automated Blood Collection System. (2015, September). Retrieved from Franks Hospital Workshop: http://www.frankshospitalworkshop.com/equipment/documents/dialysis_units/service_manuals/Terumo%20BCT%20Trima%20Accel%20Blood%20Collection%20System%20-%20Service%20manual.pdf