Osmolality and osmolarity are two closely related concepts in clinical chemistry that describe the concentration of solutes in a solution. While these terms are often used interchangeably, they have distinct definitions and applications in clinical settings. If you are asking yourself what the difference is between osmolality and osmolarity, let us discuss these key differences and how both of these analytes can assess your health status.
Basic Definitions
Osmolality: is defined as the concentration of osmotically active particles in a solution, expressed as the number of millimoles of solute per kilogram of solvent (usually water). The unit of measurement for osmolality is millimoles per kilogram (mmol/kg) or osmoles per kilogram (Osm/kg).
Osmolarity: is defined as the concentration of osmotically active particles in a solution, expressed as the number of millimoles of solute per liter of solution. The unit of measurement for osmolarity is millimoles per liter (mmol/L) or osmoles per liter (Osm/L).
Key Differences Between Osmolality and Osmolarity
The primary distinction between osmolality and osmolarity lies in the unit of measurement. Osmolality is based on the mass of the solvent (per kilogram), whereas osmolarity is based on the volume of the solution (per liter). This difference is significant in certain clinical applications. While osmolality and osmolarity are closely related, osmolality is generally preferred in clinical settings for several reasons:
Accuracy: Osmolality measurements are less affected by the presence of lipids or proteins in the sample, making them more accurate in certain clinical situations.
Temperature independence: Osmolality is based on the number of particles per kilogram of solvent, which is not affected by temperature changes. Osmolarity, being volume-based, can be influenced by temperature fluctuations.
Direct measurement: Osmolality can be directly measured using an analyzer (osmometer), while osmolarity needs to be calculated.
Physiological relevance: Osmolality more closely reflects the concentration of particles that affect fluid movement across cell membranes. Despite these advantages which osmolality possess, osmolarity still remains useful in certain situations, particularly when quick estimations are needed or when direct osmolality measurements are not available.
Reasons for Osmolality and Osmolarity Testing
Both osmolality and osmolarity measurements are useful in several ways:
Assessment of fluid/electrolyte balance: These tests help evaluate a patient’s hydration status and electrolyte balance, which are crucial for maintaining proper cellular function and overall health. They can also help guide fluid and electrolyte replacement therapy if necessary.
Diagnosis: Abnormal osmolality or osmolarity values can help diagnose a variety of medical conditions and disorders.
Evaluation of kidney function: Osmolality tests, particularly urine osmolality, can provide insights into the kidney’s ability to concentrate or dilute urine.
Detection of toxic substances: Elevated osmolal gap (the difference between measured and calculated osmolality) can suggest the presence of toxic substances like methanol or ethylene glycol which have been ingested. Unlike ethanol, these alcohols are cannot be ingested or it can cause major organ damage or death.
Normal Lab Values
Serum Osmolality: The normal range for serum osmolality is typically between 275-295 mOsm/kg.
Urine Osmolality: Normal urine osmolality has a much wider range than normal serum levels due to variance in hydration status and other factors. Generally, it ranges from 50-1200 mOsm/kg, with higher values indicating more concentrated urine. First morning urine is usually the most concentrated, with values often between 600-800 mOsm/kg. In well-hydrated individuals, urine osmolality is usually less than 800 mOsm/kg.
What Causes Low Osmolality/Osmolarity?
- Overhydration or water intoxication
- Syndrome of inappropriate antidiuretic hormone secretion (SIADH)
- Congestive heart failure
- Liver cirrhosis
- Nephrotic syndrome
- Hypothyroidism
- Addison’s disease
What Causes High Osmolality/Osmolarity?
- Dehydration
- Diabetes mellitus (especially diabetic ketoacidosis)
- Diabetes insipidus
- Hypernatremia
- Uremia (kidney failure)
- Alcoholism or alcohol intoxication
- Ingestion of certain toxins like ethylene glycol and methanol.
Sample Types and Collection Methods
Common sample types for osmolality include:
Serum or Plasma: Venous blood is drawn into a tube without anticoagulant (for serum) or with an anticoagulant (for plasma). The sample is then centrifuged to separate the cellular components from the liquid portion.
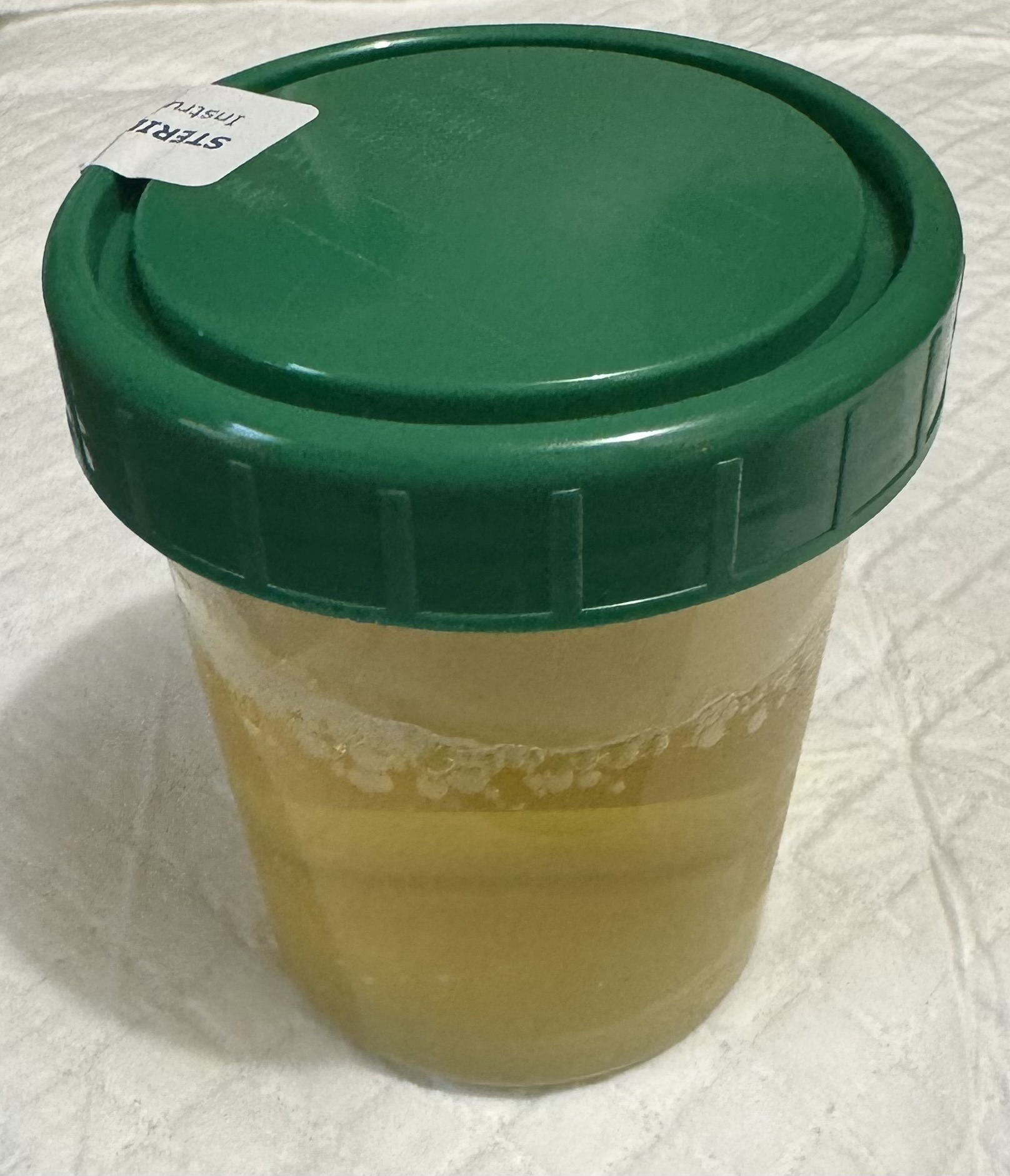
Urine: A clean-catch, midstream urine sample is usually sufficient, however, a 24-hour urine collection may be requested in certain cases.
Other fluids: In some cases, osmolality may be measured in cerebrospinal fluid, saliva, or other bodily fluids. Collection methods vary depending on the fluid type. Samples should be processed and analyzed promptly to avoid evaporation, which can affect results. If immediate analysis is not possible, samples should be refrigerated or frozen, depending on the expected delay and laboratory protocols.
Calculating Osmolarity
Osmolarity is not measured directly like osmolality, rather it is calculated based on the concentrations of sodium, potassium, glucose and blood urea nitrogen(BUN) in the blood or urine. The most common formula for calculating serum and urine osmolarity is:
Osmolarity Formula:
Osmolarity = 2[Na+K] + [Glucose]/18 + [BUN]/2.8
Found below are the normal ranges for Sodium, Potassium, Glucose and BUN. This will give you an idea of what levels are most likely to be encountered in a healthy individual. The closer that we get to the middle of these ranges, the more likely we will see a normal osmolarity result:
Normal Ranges
- Sodium- 135 to 145 mmol/L
- Potassium- 3.7 to 5.2 mmol/L or
- Glucose- 70 to 100 mg/dL
- BUN- 6 to 20 mg/dL
Osmolarity Calculation Example:
Utilizing the results of a patient’s recent Basic Metabolic Panel (BMP), calculate their osmolarity using the following results:
- Sodium- 138 mmol/L
- Potassium- 4.5 mmol/L
- Glucose- 80 mg/dL
- BUN- 11 mg/dL
Plug the patient’s results into the formula as shown below:
- 2[Na+K] + [Glucose]/18 + [BUN]/2.8
- 2[138+4.5] + [80]/18 + [11]/2.8=
- 285 + 4.44 + 3.92=
- Osmolarity= 293.36
With a calculation of 293, this patient’s osmolarity would be considered within normal ranges. As you can see by the weighting of each solute in the formula, sodium has the largest effect on osmolarity results. In fact, it can often account for over 90% of the total particles in a given solution.
What Is Osmolal Gap?
It’s important to note that calculated osmolarity may differ from measured osmolality, and this difference (Osmolal Gap) can provide valuable diagnostic information. An elevated Osmolal Gap (typically >10 mOsm/kg) can indicate the presence of various conditions with the most common being ingestion of toxic alcohols (methanol, ethylene glycol, diethylene glycol, propylene glycol and isopropanol).
Conclusion
While osmolality and osmolarity are closely related concepts, understanding their differences and appropriate applications is crucial for accurate clinical interpretation and patient care. The measurement of these parameters provides valuable insights into fluid and electrolyte balance, kidney function, and various pathological conditions.
References
- Najem, O., Shah, M. M., Zubair, M., & Jesus., O. D. (2024, February 27). Serum Osmolality. Retrieved from National Library of Medicine: https://www.ncbi.nlm.nih.gov/books/NBK567764/