Fetomaternal bleeds can occur at various points during the pregnancy journey. It’s important to detect these bleeds, also known as fetomaternal hemorrhage (FMH) as early as possible, particularly in pregnancies with Rh-negative mothers and Rh-positive babies. This is because if there has been a bleed, the mother will need to receive one or more doses of Rho(D) Immune Globulin (Rhogam) in order to prevent Anti-D antibody production and Hemolytic Disease of the Newborn (HDN). There are multiple lab tests which can detect fetomaternal bleeds in the pregnant mother. The “Rosette Test” is a qualitative method and the “Kleihauer Betke” and “Flow Cytometry” methods are quantitative methods. We will discuss the pros and cons of each of these methods in detail below.
Fetomaternal Bleed “Rosette” Screen
The Fetomaternal Bleed Screen, also known as the “Rosette” test, is usually the first test to be run when determining if fetaomaternal bleeds have occurred. It is often performed during the 28-week checkup, post-partum or any time that trauma has occurred to the mother (car accident, a fall, domestic abuse, etc).
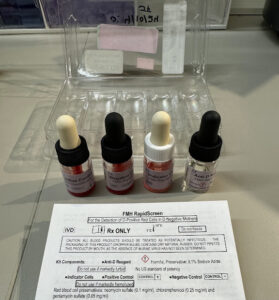
The rosette screen detects if 10 mL or more of fetal whole blood has mixed into the maternal circulation. The fetal cells must be D-positive and the maternal cells must be D-negative for the test to work. This is due to the use of Anti-D reagent which is used during the procedure. If the mother is Rh positive, then you will have an overwhelming false positive result since the Anti-D reagent will bind to the Rh-positive red cells as they are in essence mimicking the activity of a Rh-positive baby. This is why running a rosette test on a Rh-positive mother is not necessary and is a waste of time and resources. This test should only be performed on Rh-negative mothers.

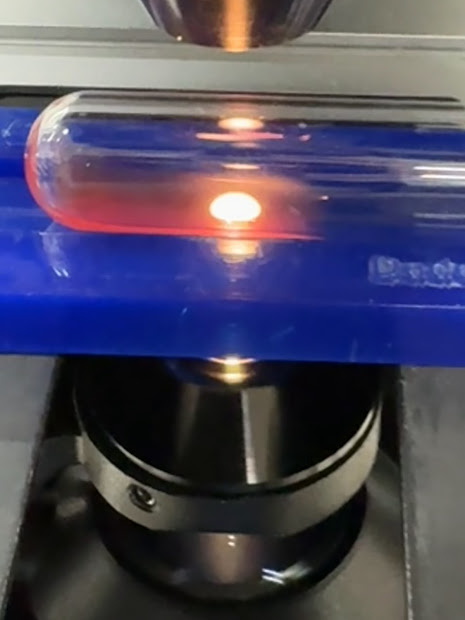
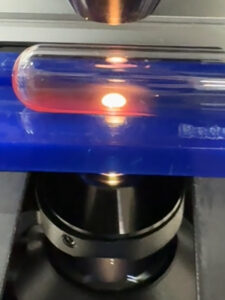
In the rosette screen, a maternal blood sample is incubated with anti-D and then washed. Indicator Rh-positive RBCs are added and the sample is then examined under a microscope. If Rh-positive fetal cells are present, the indicator cells will form aggregates resembling “rosettes” around the fetal cells. If 5 or more of these rosettes are seen after examining five low-power fields, this is considered a positive screen. This number may be more or less depending on the method being used.

If the rosette test is negative, one vial (300 μg) of Rhogam is administered immediately. If the rosette test is positive, one vial (300 μg) of Rhogam will still be administered immediately, but the blood sample must also be sent for quantitative testing in order to determine the severity of the bleed. The results of this testing will determine if any additional doses of Rhogam should be given and how many vials would be appropriate to give.

Pros: Fetomaternal Bleed “Rosette” Screen
1. Inexpensive. Only requires an Fetomaternal Bleed Screeing kit and a microscope.
2. Easy to perform.
3. Can be conducted around the clock. Turnaround time in 1-2 hours.
Cons: Fetomaternal Bleed “Rosette” Screen
1.Since it relies on the presence of the D antigen to distinguish fetal from maternal cells, it cannot be used to detect bleeds in Rh-positive mothers, or Rh-negative mothers who are carrying a Rh-negative fetus.
2. Will only alert you if there was a bleed (qualitative), but it won’t tell you how severe it was (quantitative).
Kleihauer-Betke Test
The Kleihauer-Betke acid-elution test is the most commonly used test for quantifying fetomaternal bleeds. It relies on the fact that fetal RBCs contain mostly fetal hemoglobin (HbF), which is resistant to acid-elution whereas adult hemoglobin (HbA) is acid-sensitive.
This is the reason that when a smear of maternal blood is exposed to an acid buffer, the hemoglobin from the adult red cells will be removed while the hemoglobin F in the fetal red cells will be retained. To help visualize the difference in appearance between the adult and fetal cells, the slide will be dyed with a stain, causing the fetal cells to turn pink while the maternal cells will be stay pale, earning them the name “ghost cells”.
The number of additional Rhogam vials is calculated by determining the % of fetal cells per 2,000 total cells counted. Once the % of fetal cells is identified, multiply it by 50 and divide by 30.
If the number to the right of the decimal is less than 5, round down and add 1 vial.
If the number to the right of the decimal is greater than or equal to 5, round up and add 1 vial:
Example: If 1.7% of the 2,000 total cells counted were identified as fetal cells (stained pink).
Volume of fetal blood which has mixed into maternal circulation: 1.7 x 50 = 85 mL
Number of Rhogam vials: 85 mL/30 = 2.83 (round up to 3 and add 1 more)
In this example, it takes 4 vials of Rhogam to prevent Anti-D sensitization from 85 ml of fetal blood.
Pros: Kleihauer-Betke
1. Inexpensive. Only requires a KB staining kit and a microscope.
2. Gives a quantitative estimate of bleed severity. Helps guide additional Rhogam dosing.
3. Doesn’t rely on the presence of the D antigen to distinguish fetal from maternal cells, therefore, it can be used to detect bleeds in Rh-positive mothers and Rh-negative mothers who are carrying a Rh-negative fetus.
Cons: Kleihauer-Betke
1. Time consuming and tedious. Must manually count each cell one by one.
2. Usually only performed at larger facilities. Often requires ship-out, causing extended turnaround times. Not typically done around the clock.
3. Accuracy and precision can suffer due to procedural variation (smear preparation, interpretation can be subjective between different technicians).
4. Conditions like sickle cell anemia and others which cause elevated HbF cells in adults will skew results.
Flow Cytometry
Flow cytometry is another method of quantifying fetmomaternal bleeds. Like the Kleihauer Betke test, flow cytometry also utilizes fetal hemoglobin (HbF), although in a different way. Instead of using HbF directly, it uses antibodies to bind to the HbF inside of the red blood cells. The antibody tagged cells can then be identified as fetal cells as they move through a flow cytometer during analysis.
Pros: Flow Cytometry
1. Gives a quantitative estimate of bleed severity. Helps guide additional Rhogam dosing.
2. Doesn’t rely on the presence of the D antigen to distinguish fetal from maternal cells, therefore, it can be used to detect bleeds in Rh-positive mothers and Rh-negative mothers who are carrying a Rh-negative fetus.
3. Speed of analysis. Automation allows a greater number of cells to be counted in less time than the manual method of Kleihauer Betke.
4. Has greater reproducibility (precision) since the analyzer is more standardized than human technicians who may be subjective. Doesn’t have the accuracy and precision issues that the Manual KB test has.
Cons: Flow Cytometry
1. Equipment is expensive.
2. Less trained staff available since flow cytometry is a highly specialized area of the lab.
3. Not widely utilized. According to 2009 CAP surveys, less than 5% of labs reported using flow cytometry as a method1. Usually only performed at large facilities or reference labs and often requires ship-out, causing extended turnaround times. Not conducted around the clock.
Impact of Testing for Fetomaternal Bleeds
Detecting a fetal bleed early on is crucial, particularly in Rh-negative mothers who have Rh-positive babies. If fetomaternal bleed testing is not carried out properly, a mother could potentially get less of a Rhogam dose than she should, opening up the risk of developing Hemolytic Disease of the Newborn, a condition that is often fatal.
Conclusion
The Rosette test is useful for detecting fetomaternal bleeds, but only for Rh-negative mothers due to its reliance on Anti-D.
Kleihauer Betke and Flow Cytometry are able to quantify bleeds and gauge Rhogam dosing without reliance on Anti-D, rather with fetal hemoglobin.
Flow cytometry is the future of fetomaternal bleed testing due to its superior accuracy, precision and speed. However, the cost of equipment and limited staffing will keep it sparsely available in only a select few labs. Until then, the KB stain will remain the chosen quantitative method for years to come.
References
1. Yeowon A. Kim, R. S. (2011, November 16). Detection of Fetomaternal Hemorrhage. Retrieved from American Journal of Hematology: https://onlinelibrary.wiley.com/doi/full/10.1002/ajh.22255