Cotinine testing has become an important tool for individuals, healthcare providers and companies to assess exposure to nicotine, whether from direct use or secondhand smoke. Initial screening is often done using at-home nicotine (cotinine) test kits and confirmation of presumptive positives are usually performed in an accredited laboratory. In this article, we will focus on the basics of the at-home side of testing and will explore the reasons for testing, cotinine preference over nicotine, sampling options, testing methods, result interpretation, baseline levels, detection limits and factors affecting testing.
Why Is Cotinine Tested Instead Of Nicotine?
Cotinine is the primary metabolite of nicotine. When a person consumes nicotine through smoking, vaping, dipping, or other methods, the body breaks down the nicotine into cotinine. So why is cotinine tested for instead of nicotine? The main reason is that cotinine has a longer half-life than nicotine (15-20 hours compared to nicotine’s 0.5-3 hours)1, making it easier to detect nicotine use for longer periods. Another reason is that cotinine is less affected by pH levels in the body than nicotine.
Reasons for Cotinine Testing
Secondhand Smoke Exposure: Non-smokers concerned about their exposure to secondhand smoke can use cotinine tests to determine if they are being affected. This is particularly important for parents of young children or individuals with respiratory conditions.
Insurance Purposes: Some insurance companies offer lower premiums for non-smokers. Cotinine tests may be required to verify an individual’s non-smoking status before they can lock in rates for a new policy.
Employment Screening: Certain employers, particularly in healthcare or safety-sensitive industries, may require cotinine testing as part of their pre-employment screening or ongoing employee health assessments. Many employers do not allow tobacco or other forms of nicotine in the workplace or at home, so a negative test is required upon on-boarding and must be maintained throughout the employment period.
Self-Reported Smoking Status: In healthcare settings, cotinine tests are sometimes needed to verify that a patient is not using nicotine prior to certain medical procedures like surgery. Nicotine use can cause reduced blood flow and increase the risk for infection.
Sometimes, people want to check themselves prior to testing for one of the above purposes. By using at-home cotinine tests, they can get an idea if they are below the standard cutoff of 200 ng/mL.
Specimen Types for At-Home Cotinine Testing
Urine: Urine is the most common specimen used for at-home testing. This is due to its non-invasiveness and ease of collection. However, some drawbacks to urine testing are that you must drink a lot of water prior to the test to ensure you can urinate. Also, some urine-based kits don’t come with a urine cup, so one must be sourced externally, adding an extra step to the process.
Saliva: Some companies have started making saliva-based test kits, although they are still not very common. With saliva-based kits, the mouth is swabbed and then the test is run. No urine cups or restrooms needed. One thing to keep in mind though is that some saliva-based kits may require no eating or drinking prior to the test, due to the potential for false results.
Blood: If confirmation of a preliminary positive at-home test is desired, blood specimens can be drawn for testing. However, this testing requires a trip to the hospital to get blood drawn by a trained phlebotomist and requires the sample to be run on a Gas or Liquid Chromatography Mass Spectrophotometer in an accredited laboratory. This may require an order from a doctor.
For the purposes of this article, we’ll focus primarily on urine and saliva testing, since these are the methods used for at-home testing.
Methodology for At-Home Cotinine Testing
At-home tests typically use immunoassay technology to screen for the presence of cotinine in body fluids like urine and saliva. When the absorbent end of a test device is immersed into a specimen, the liquid is absorbed via capillary action, mixes with conjugate before flowing across a pre-coated membrane. Any cotinine that is present in a sample will bind to monoclonal antibody binding sites and will cause either one- or two-colored lines to become visible, depending whether cotinine levels are above or below the cutoff level for that kit.
Factors Affecting Cotinine Levels
Several factors can influence cotinine levels in the body and should be considered when interpreting results:
Metabolism: Individual variations in metabolism can affect how quickly cotinine is cleared from the body, particularly the functioning of organs like the kidneys. If the kidneys are not filtering the blood as they should, excessive cotinine levels could build up, making it more likely that a test will be positive.
Hydration: Well-hydrated individuals may have more dilute urine, potentially leading to lower cotinine concentrations. Those that are dehydrated will have more concentrated urine, making a positive result more likely. Urine samples are also more concentrated in the morning, making a positive result more likely.
Time since last use/exposure: Cotinine levels decrease over time after nicotine exposure stops.
Frequency and intensity of nicotine use: Heavy smokers will generally have higher cotinine levels than light or occasional smokers.
How Much Cotinine Do Nicotine Users Typically Have In Their System?
Cotinine levels are usually measured in nanograms per milliliter (ng/mL). The interpretation of results can vary slightly depending on the specific test and manufacturer, but general guidelines are as follows:
Cotinine levels in a nonsmoker are generally less than 10 ng/mL. Cotinine levels in a light smoker or someone exposed to secondhand smoke are 11 ng/mL to 30 ng/mL. Cotinine levels in a heavy smoker may be more than 500 ng/mL2.
The cutoff for a positive result is typically around 200 ng/mL for urine tests and 30 ng/mL for saliva tests.
How Long Can Cotinine Be Detected?
After cessation of smoking cotinine concentrations should decline to nonsmoking levels within 4 days in the majority of cases, with an upper limit of 7 days. Nonsmoking levels are considered < 10 ng/ml in plasma and saliva and < 50 ng/ml in urine3.
The length of time that cotinine remains detectable in the body depends on various factors, so keep in mind that these are approximate timeframes and can vary between individuals.
Interpreting Test Results
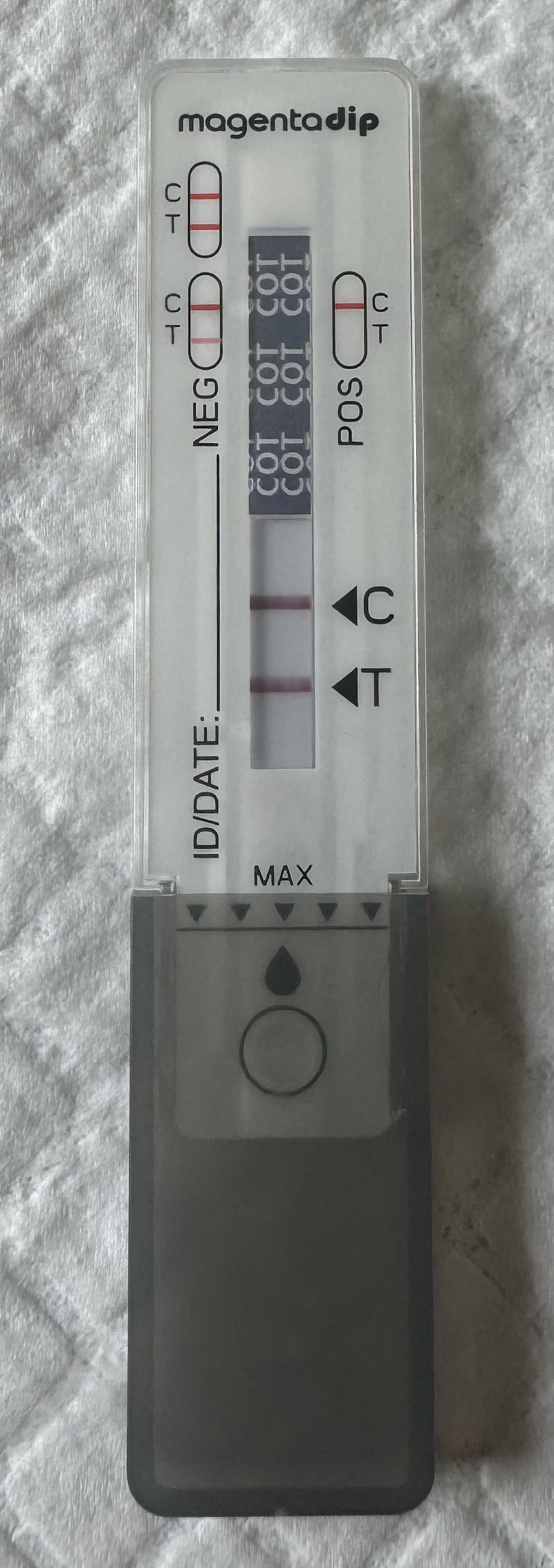
Negative Result: Indicates no significant nicotine exposure in the recent past. This could mean you’re a non-smoker or that it has been long enough since your last nicotine use or exposure for cotinine levels to drop below the test’s detection threshold. A colored band will be visible in the Control Region (C) and the Test Region (T) causing 2 lines to be seen.
Positive Result: Indicates recent nicotine exposure, either from direct use or secondhand exposure. However, tests cannot distinguish between these sources. A colored band will be visible in the Control Region (C), but no colored band will appear in the Test Region (T), causing only 1 line to be seen.
Invalid: If a colored band is not visible in the Control Region (C), the test is deemed invalid, even if a line still shows up in the Test Region (T). Another test should be run to re-evaluate the specimen. If the test still fails, contact the manufacturer for further guidance.
The color intensity of control and test region lines do not always signify a weak positive or negative, nor a strong positive or negative. Thus, a preliminary positive result does not always mean that a person has used nicotine and a negative test result does not always mean that a person hasn’t used nicotine. There could be a number of factors that affect the strength of a result.
Limitations of At-Home Cotinine Testing
While at-home cotinine tests can be useful tools, they have some limitations:
Qualitative results: Most at-home tests only provide positive/negative results, not specific (quantitative) cotinine concentrations.
Potential for false positives: Certain foods have naturally occurred nicotine, so they can potentially cause false positives if large amounts are ingested, although unlikely. Foods like tomato, potato, black tea and instant tea have wet weight concentrations of 7.3 ng/g, 15 ng/g, > 100 ng/g and up to 285 ng/g, respectively4.
Unable to distinguish source: Positive results could be from active smoking, passive exposure, or nicotine replacement therapy (gum and patches). Testing will not be able to differentiate the method of intake.
User error: Improper sample collection or test administration can affect results.
Ensuring Accurate Results
To maximize the accuracy of your at-home cotinine test:
- Avoid contamination: Ensure the sample and test components don’t come into contact with anything that could affect the results.
- Check expiration dates: Don’t use expired test kits.
- Store properly: Keep test kits at the recommended temperature and away from direct sunlight, moisture and heat. Do not ever put test kits in the freezer.
- Test should be performed at room temperature 18ºC-30ºC (65ºF-86ºF).
- Test kits are only validated to run one type of specimen. So, if you are using a urine kit, only test a urine specimen, not saliva. Likewise, when using a saliva test kit, do not use urine. Not using the appropriate specimen for a test kit can cause inaccurate results.
At-Home Cotinine Testing And The Road To Recovery from Nicotine
At-home cotinine testing can be a valuable tool for individuals monitoring their smoking cessation progress, assessing secondhand smoke exposure and verifying non-smoking status.
If you are struggling with smoking cessation, consult with a healthcare provider. They can provide more comprehensive testing if needed and offer support and resources to help you achieve your health goals.
As our understanding of the health impacts of nicotine and tobacco use continues to evolve, tools like cotinine testing will likely play an increasingly important role in both personal health management and public health initiatives.
References
1.Cotinine and Hydroxycotinine – Serum (COT_I). (2019, April). Retrieved from CDC: https://wwwn.cdc.gov/Nchs/Nhanes/2015-2016/COT_I.htm
2.Nicotine Cotinine (Urine). (2024). Retrieved from University of Rochester Medical Center: https://www.urmc.rochester.edu/encyclopedia/content.aspx?contentid=nicotine_cotinine&contenttypeid=167
3.Martin J. Jarvis, M. M. (1988, June). Elimination of Cotinine from Body Fluids: Implications for Noninvasive Measurement of Tobacco Smoke Exposure. Retrieved from National Library of Medicine: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1350287/pdf/amjph00245-0090.pdf
4.Davis, R., Stiles, M., deBethizy, J., & Reynolds, J. (1991). Dietary nicotine: A source of urinary cotinine. Food and Chemical Toxicology, 821-827. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/027869159190109K?via%3Dihub