Published: 11 September 2023
Donating Plasma Overview
Donating plasma is a great way to make some money, but its an even better way to save someone’s life. According to Western Michigan University, plasma centers in the United States received a record 53.5 million plasma donations in 2019 across roughly 900 donor facilities. These units are sought after for use both in hospital patient care as well as research. However, for as many reasons there are to roll up your sleeve and donate, there are also many reasons why one should not donate. I’ve previously worked in a blood donor center, so I have firsthand experience in dealing with donors that have disqualifying conditions. Let’s discuss 25 of the top reasons why you shouldn’t donate plasma or other blood products, when considering common disqualifications.
Donor Interview
Before you are approved for donation, medical screening must be performed at the plasma center. The staff will ask you a series of interview questions to help determine if your medical history would produce a safe unit of blood for a recipient. In some facilities, the interview process may be automated or semi-automated. The following numbered items include various categories of conditions that deem a person ineligible as a blood donor in accordance with the 2023 version of the AABB Blood Donor History Questionnaire Form DHQ v4.0.
1. General Health
If you are not feeling well on donation day, you should not donate until you are feeling better, even if it’s just a common cold. This is to prevent possible transmission of infectious diseases to the recipient.
2. Antibiotics; Active Infections

You should not be taking any antibiotics or other medications for an infection. If you are, the donor staff will ask why you are taking them and will need to determine if you have a bacterial infection that could be transmissible by blood. If you have an active infection, you should not donate.
3. Pregnancy
If you are currently pregnant, you shouldn’t donate. You must wait 6 weeks after delivery to donate again. Once the deferral period has passed, they may donate again, but if donating whole blood, their plasma will not be eligible for manufacture into Fresh Frozen Plasma (FFP) due to Transfusion-Related Acute Lung Injury (TRALI) risk. At the donor center that I worked at, we turned these units into Recovered Frozen Plasma instead of FFP, to prevent wastage.
4. Medications
Some medications have the potential to compromise your safety as the donor as well as the recipient. So certain drugs on the Medication Deferral List should defer a donor for the appropriate time frame.
- Antiplatelet agents affect platelet function, so people taking these drugs should not donate platelets. Deferral times are as follows. Feldene and Aspirin: 2 days, Effient: 3 days, Brilinta: 7 days, Plavix: 14 days, or Zontivity: 1 month.
- Anticoagulants or “blood thinners” like Coumadin are used to treat/prevent blood clots and to prevent strokes. However, these medications affect the donor’s clotting abilities and can cause excessive bruising or bleeding when you donate. Deferral periods are 2 days from the last dose for Arixtra, Eliquis, Fragmin, Lovenox, Pradaxa, Savaysa and Xarelto and 7 days from the last dose for Coumadin and Heparin.
- Popular acne treatments like Isotretinoin (Accutane) trigger a 1-month deferral from the last dose.
- Multiple Myeloma treatments Thalomid (Thalidomide) and Revlimid (Lenalidomide) incur 1-month deferrals.
- Rheumatoid Arthritis medication Rinvoq (Upadacitinib) is 1 month deferred.
- Hair loss remedy Propecia (Finasteride) is 1 month deferred.
- Immunosuppressant medication Cellcept (mycophenolate mofetil) can cause birth defects or death of an unborn baby if transfused to a pregnant recipient. This will be a 6-week deferral.
- Hepatitis B Immune Globulin (HBIG) is injected to prevent hepatitis B infection following a possible or known exposure. Those receiving HBIG must wait 3 months from their last dose to donate plasma.
- HIV prevention PrEP involves taking oral medicines or injections as a prevention effort for HIV negative people at high risk of HIV infection. PEP or post-exposure prophylaxis is a short-acting treatment started as soon as possible after a high-risk exposure to HIV to reduce the risk of infection. Truvada and Descovy will incur a 3-month deferral, whereas Apretude will be a 2-year deferral.
- Basal Cell Skin Cancer medications Erivedge and Odomzo are 2-year deferrals.
- Multiple Sclerosis drug Aubagio is a 2-year deferral.
- Rheumatoid Arthritis drug Arava is a 2-year deferral.
- Psoriasis drug Soriatane is a 3-year deferral.
- Psoriasis drug Tegison is a permanent deferral.
- Antiretroviral Therapy (ART) medications to treat HIV are a permanent deferral.
- Experimental medications are usually associated research studies, so their deferral periods will vary as defined by guidance given by the medical director.
5. Donation Frequency

You may donate a unit of red blood cells no more frequently than every 8 weeks. If you have donated a double unit of red blood cells using an apheresis machine, that time is extended out to 16 weeks. For plasma, platelets or granulocytes by apheresis, donors can donate at a maximum of twice a week, with at least 24 hours between visits.
6. Vaccinations

Vaccines are important in preventing various diseases, but they can disqualify you from donating blood. Smallpox is one of the major ones as it requires a 56-day deferral period after someone receives the shot. There is also a deferral period for those who have been around someone who has had the shot in the past 8 weeks. That person should be deferred for 56 days from the current date or 14 days from the resolution of complications, whichever is later.
7. Anal Sex
A person who has had sexual contact with a new partner or multiple partners in the past 3 months and who has also had anal sex in the past 3 months is at increased risk of transmitting HIV infection and other infectious diseases. Consequently, a donor is deferred for 3 months from their last date of anal sex or 3 months from the date of the current donation attempt if they don’t recall their last date of anal sex.
8. Other Sexual Contact
Sexual Contact is defined as either vaginal, or anal sex.
- If someone has sex with a person that has ever had a positive test for HIV, they are deferred for 3 months from the last sexual contact.
- If someone has received money, drugs or other payment for sex, they are deferred for 3 months from the last payment. If you have sex with somebody else who has received money, drugs or other payment for sex, they are deferred for 3 months from the last sexual contact.
9. IV Drug Abuse
- A person who has used needles, in the past 3 months, to inject drugs, steroids, or anything not prescribed by their doctor is deferred for 3 months.
- In the past 3 months, if a person has had sexual contact with anyone who had used needles in the past 3 months to inject drugs, steroids, or anything not prescribed by their doctor, they are deferred for 3 months from the date of last sexual contact.
10. STDs
If in the past 3 months, if a person had syphilis or gonorrhea or was treated for it during that time, they are deferred for 3 months after the date treatment was completed.
11. Hepatitis
If in the past 3 months, if a person had sexual contact with someone who has viral hepatitis, particularly Hepatitis B, symptomatic Hepatitis C, or unknown types, they are deferred for 3 months from the date of last sexual contact. Additionally, if a person has lived with someone with this type of hepatitis in the past 3 months, they are deferred for 3 months from the last date of living there.
12. Blood Exposure
If a person is exposed to someone else’s blood via contact with an open-wound, non-intact skin, or mucous membrane; or if they encounter an accidental needlestick, they will be deferred for 3 months from the date of exposure.
13. Tattoos

If a person has had a tattoo in the past 3 months, they are deferred for 3 months from the date of the tattoo application unless it was applied by a state regulated entity with sterile needles and single-use ink. Tattoos include permanent makeup like eyeliner, lipliner, & microblading as well.
14. Piercings
If a person has had an ear or body piercing in the past 3 months, they are deferred for 3 months unless it was done using single-use equipment.
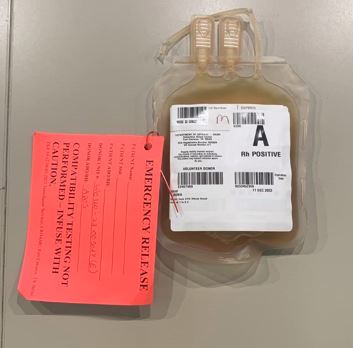
15. Prior Transfusions
A person who has received an allogeneic blood transfusion (blood from someone else) is deferred for 3 months following the transfusion. This does not apply to autologous transfusions where someone receives their own blood from a previous donation.
16. Transplants/Grafts/Dura Mater
If someone has an organ, tissue, or bone marrow transplant, they will be deferred for 3 months following the procedure. There is also a 3-month deferral after any bone or skin graft procedure. A person who has ever received an allogeneic dura mater transplant or graft is permanently deferred. Autologous dura mater grafts are acceptable.
17. Incarceration
If a person has been in juvenile detention, lockup, jail, prison, or a correctional facility of any type for 72 consecutive hours within the past 12 months, they will be deferred for 12 months from the date of release.
18. Travel History/Malaria Risk

Traveling to malaria-endemic countries is a common occurrence which can prevent donor eligibility. Several factors like being a prior resident of an endemic country or not, length of stay during the travel and which blood product is being targeted all determine the length of deferral. This will either be 3 months or 3 years from the time of departure.
19. Malaria Infection
Malaria causes a severe and often fatal disease which is caused by the Plasmodium parasite. If someone has ever been infected with malaria in their life, they are deferred for 3 years after becoming asymptomatic if while living in a non-endemic country.
20. HIV History
If a person has ever tested positive for HIV and it was confirmed to be positive, they will be permanently deferred for life.
21. Cancer
If a person has ever had any type of cancer or leukemia, they may be deferred for a period of time dependent on the individual facility SOP.
22. Heart and Lungs
If a person has ever had any heart or lung problems, they may be deferred for a period of time dependent on the individual facility SOP.
23. Bleeding Conditions
If a donor has ever had a bleeding condition or blood disease, this may be grounds for a deferral. If it is hemophilia or a related disorder, it will be an indefinite deferral. What is the difference between an indefinite and permanent deferral? An indefinite deferral means it is for an unspecified period of time, as opposed to a permanent deferral which is forever. With indefinite deferrals, there is at least a chance for the person to donate in the future if the rules change. With permanent deferrals, there is no chance even if the rules change.
24. Babesia

Babesiosis is a rare red blood cell disease caused by the bite of a tick infected with the parasite Babesia microti. If a donor has ever tested positive for Babesia, they will be deferred and will be eligible for requalification testing after at least 2 years following the date of the most recent reactive test result.
25. Vitals/Physical Exam Requirements
If the donor makes it through the interview process, they must meet the following physical exam and vitals requirements in accordance with 21 CFR Part, 630.10:
- Age: must be 16 years or older.
- Weight: must weigh at least 110 pounds.
- Arm check: The phlebotomy site in the antecubital area should be free of infection, inflammation and lesions. Donor center staff will check your arms for evidence of IV drug use and other abnormalities.
- Blood Pressure: the systolic must be between 90-180 mm Hg and the diastolic must be between 50-100 mm Hg. If outside of these levels, approval by the medical director will be required to ensure the donor’s health won’t be affected by donating.
- Pulse: the pulse should be between 50-100 beats per minute. Medical Director approval will be necessary if donor is outside of these limits, to ensure that the donor’s health won’t be affected.
- Temperature: must be less than or equal to 37.5 C (99.5 F).
- Hemoglobin: Males must have a hemoglobin of 13.0 g/dL or higher and females must have a hemoglobin of 12.5 g/dL or higher.

Donor File Review, Phlebotomy & TTD Testing
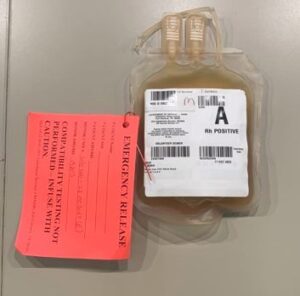
If a donor makes it past the interview and vitals process, they will typically go thru one last final check to ensure their donor file is complete and void of any errors before they are sent back to phlebotomy to have the unit drawn. Once the process is complete, the unit still cannot be released since Transfusion Transmitted disease (TTD) testing must be performed first. The vacutainer tubes that are drawn during the phlebotomy are sent to a lab to be tested for common infectious diseases like: HIV Types 1 and 2; Hepatitis B virus; Hepatitis C virus; Human T-Lymphotropic Virus Types 1 & 2; Treponema Pallidum (Syphilis); West Nile Virus; Trypanosoma Cruzi (Chagas Disease); Variant Creutzfeldt-Jakob disease (vCJD, Mad Cow Disease); and Plasmodium (Malaria). If any tests come back positive, the unit will then be quarantined & destroyed. Likewise, the donor will be deferred accordingly for any donations in the future. At the donor center I worked at, we would keep these units in a pending fridge after the blood drive until the testing results came back early the next day, after which we would ship those units off to the hospital.
Conclusion
Donating plasma can be a good way to help the medical community while simultaneously making money. However, there are many ways to become disqualified from the process due to the strict regulatory requirements for prospective blood donors.
References
21CFR, 630.10. (2023, June 07). Retrieved from Food & Drug Administration: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/cfrsearch.cfm?fr=630.10#:~:text=The%20donor%27s%20pulse%20must%20be,(5)%20Weight
AABB. (2023, May 11). Blood Donor History Questionnaires. Retrieved from Association for the Advancement of Blood & Biotherapies: https://www.aabb.org/docs/default-source/default-document-library/resources/dhq-v4-0/pdfs/dhq-v4-0-flowcharts.pdf?sfvrsn=aa096c03_6
Ochoa, A., Shaefer, H. L., & Grogan-Kaylor, A. (2021, June). The Interlinkage between Blood Plasma Donation and Poverty in . Western Michigan University- The Journal of Sociology & Social Welfare, 48(2), 4. Retrieved from https://scholarworks.wmich.edu/jssw/vol48/iss2/4